DOI: 10.26717/BJSTR.2023.52.008250
National University of Physical Education and Sports, Faculty of Physical Education and Sport, Romania.
*Corresponding author: Alexandra Tufa, National University of Physical Education and Sports, Faculty of Physical Education
and Sport, Bucharest, Romania
Received: February 15, 2023
Published: August 23, 2023
Citation: Alexandra Tufa and Silvia Te-
odorescu. Physiotherapy Management
of Urinary and Fecal Incontinence in a
Nulliparous Young Athlete Treatment.
A Case Report. Biomed J Sci & Tech Res
52(3)-2023. BJSTR. MS.ID.008250.
Introduction: Urinary and fecal incontinence have a major impact from an ecological, economic, health point of view. Consequent reduced quality of life through urinary tract infections and skin conditions deeply affects the patient both psychologically and socially.
Objectives: To describe the pelvic floor physiotherapy treatment in a complex case of a nulliparous young athlete who suffered of urinary and fecal incontinence after two hemorrhoidectomies.
Clinical Case: This case report presents a young nullipara athlete woman of 30 years old with urinary and fecal incontinence associated with rectal prolapse stage two and bladder prolapse stage one after two hemorrhoidectomies in 2015 and 2018. She used to practice high-impact sports: badminton and horseback riding since her eight years old. The physiotherapy consisted in learning the perineal contraction and the perineal lock during perineal high risk physical activities, electrotherapy stimulation and biofeedback, hypopressive abdominal reinforcement and behavior advice.
Conclusion: The results reveal that urinary incontinence disappeared, the fecal incontinence is improved, significant increase of perineal muscle contraction and improvement of quality of life. In conclusion physiotherapy is an efficient treatment for urinary and fecal incontinence for a nulliparou
Urinary incontinence is a real global public health challenge. The International Continence Society has defined urinary incontinence as the involuntary loss of urine that is both objectively demonstrable and a social or hygiene problem. Fewer than 30% of women with fecal incontinence seek care, and lack of information about effective solutions is an important barrier for both patients and health care professionals. Even among women with both urinary and fecal incontinence presenting for urogynecologic care, the rate of verbal disclosure of fecal incontinence symptoms remains low [1]. The goal of this study was to describe the pelvic floor physiotherapy treatment in a difficult case of a nulliparous young athlete who complained of urineand fecal incontinence following two hemorrhoidectomies. We intend to test if physiotherapy is an efficient treatment for urine and fecal incontinence for a nulliparous young athlete. In 2009, (Lasserre, et al.[2]) estimate that urinary incontinence in the French female population reaches a percentage of 26.8%, of which 34.5% in women aged between 60-69 years, 34% in women aged between 70-79 years and 46.6% in those of over 80 years. Of all the women surveyed, 60% of them have never consulted a doctor for incontinence, and 48% declare that they wear absorbent pads all the time. The incidence in women has been reported to be over 50% [3,4], with the likelihood of pregnancy significantly increasing the risks of urinary incontinence. Among female athletes, it has been shown that there is an increased percentage of urinary incontinence, which is often not reported to the coach, parents, or doctor. Following several studies, the percentage of stress urinary incontinence among sportswomen can reach a ratio between 28% and 80%. The sports with the highest risk are those requiring repeated impacts with the ground: trampoline, gymnastics, hockey, ballet, jumping, etc. [5-8]. Female performance athletes practicing trampoline jumping have been shown to report the highest prevalence of urinary incontinence, 80% [9]. Also, female athletes have an increased percentage of emergency incontinence due to bladder hyperactivity, especially in sports such as cycling or football [7]. The occurrence of this condition is, in most cases, of multifactorial origin, its treatment being complex. Even though there is an increase in the percentage with age, this disability can affect all ages.The medico-social consequences are considerable: the difficulty of schooling in children, the shame and the decrease in the quality of life and self-esteem in adults, the need to institutionalize the elderly. Also, vesico-sphincteric disorders represent the main handicap of patients with severe neurological disorders such as multiple sclerosis, spinalcord trauma, Parkinson’s, etc. Although it is such a common condition, many women suffer from urinary incontinence and hesitate to seek help from a specialist. The belief that urinary incontinence is a natural process of aging or a consequence of repeated births, combined with embarrassment, discourages them from seeking professional help. In the absence of adequate treatment, the patient limits her physical activities, social and professional life, and her sex life deteriorates. Due to the fear that urination may occur in embarrassing situations, the patient may develop anxiety or depression, low self-esteem and significantly low quality of life [10].
Management in the treatment of incontinence includes behavioral treatment, physical therapy by strengthening the pelvic floor muscles, medication or even surgical treatment in some situations. (Fantl, et al. [10]) suggested that in treatment management, as a rule, the first choice should be the least invasive method with the fewest adverse effects and complications for the patient. In this context, behavioral and pelvic floor muscle training techniques meet these criteria for most forms of urinary incontinence [11-13]. Urinary and fecal incontinence have a major impact from both an ecological, economic, health point of view through urinary infections [14] and skin conditions [15], but also psychologically and socially through decreased quality of life [16-18]. Even though most PPE manufacturers are trying to become more and more eco-responsible, the manufacture and large-scale use of PPE has a non-negligible impact on the planet. The economic impact of UI is quite difficult to estimate, first of all, due to the lack of a real percentage of the incidence of this condition, of the direct costs (the cost of medical and therapeutic consultations, the costs of hospitalizations, absorbent protections…) and secondly because of the indirect costs of incontinence: absenteeism and performance at work, psychological disorders, depression [19,20]. In France, the economic impact of UI in 2006 through the cost of protections sold in pharmacies and shopping centers was 170 million euros, with an annual increase between 8 and 15% [21]. In the United States, the total cost of overactive bladder in 2007 was estimated at $65.9 million, with a projected increase in 2015 to $76.2 million and $82.6 million in 2020 [22]. Fecal incontinence is defined as the involuntary loss of rectal contents through the anal canal and the inability to delay a bowel movement until it is socially convenient. A time and age component of at least one month and an age of at least 4 years with previousl previously achieved bowel control are attached to the definition [23,24].
1. Passive incontinence (involuntary discharge without anyawareness);
2. Urge incontinence (emptying despite active attempts to retain contents);
3. Fecal seepage [25].
The aim of this work is that the recovery program based on physical exercises and physiotherapy techniques of a nulliparous young athlete with urinary and fecal incontinence will help to increase the force of perineal muscle contraction, improve symptoms and increase
This study is a qualitative observational study of a 32-year-old female athlete with urinary and fecal incontinence associated with a prolapse occurred in 2018 following hemorrhoid surgery. The patient had already had a similar operation in 2015, but without secondary incontinence or prolapse. The study was carried out in Mions (France), between September 2021 and April 2022.
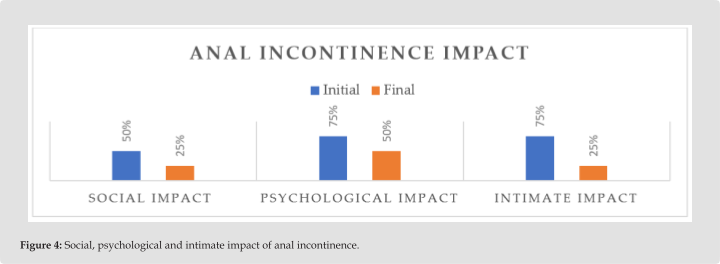
History and Clinical Examination: A 32-year-old patient presents herself to the office on 09/14/2021 with a medical prescription from her family doctor. Since the date of the prescription on 25/06/2021, the patient searched for 3 months for an office specialized in perineal recovery, this specialization being little addressed by physiotherapists. The patient complains of urinary and fecal incontinence since 2018 following a hemorrhoid surgery. She was operatedon in two stages for hemorrhoids in 2015 and 2018, but the first intervention was without complications. Following the second post-operative report from 2018, the doctors reported that this intervention would not have a direct impact on the patient’s urinary, fecal, or prolapsed incontinence, but was only a triggering element of several factors: sports – horse riding, badminton ; professional environment – the patient has been working for several years in a parcel center, often lifting heavy packages; smoking – the patient smokes more than 20 cigarettes a day since the age of 22. Also, a trigger can be an intolerance to a drug administered post-operatively with severe side effects: abdominal pain, severe vomiting and diarrhea. Severe vomiting could have triggered a sudden hyperpressure on the pelvic floor, thus causing deformations and dysfunctions and statics of the pelvic floor. The patient has lost her job, which causes serious financial problems, has had sexual problems, suffers from depression and even recently applied to the insurance company to be recognized as a disabled person. The patient states the following: she has a daily fecal incontinence, stage 2 stress urinary incontinence with a frequency of 2, 3 times a week, an urge urinary incontinence with daily urinary urges, often occurring with urinary leakage depending on the conjuncture or the situation, if the patient can reach the toilet in time.All these symptoms have important social (66%), psychological (99%) and intimate (99%) consequences.
1. MRI: anterior rectocele grade I-II, cystocele grade I (examperformed in 2018);
2. Normal recto-anal manometry in 2019;
3. Normal endo-anal ultrasound, with integrity of the internal and external anal sphincter in 2019;
1. Good abdominal tonicity;
2. Lack of automatic contraction/perineal blockage during abdominal hyperpressures or efforts (coughing, sneezing, lifting objects, sports, etc.);
3. No spinal pathologies or pain;
4. Abdominal response to coughing with a value of 0: the abdomen contracts isometrically, when coughing, a slight push is
felt towards the therapist’s hand, but at the end of the movement the abdomen returns;
5. Vulva with a normal tonicity;
6. Vaginal touch: normal tonicity, slight pain during testing;
7. Vaginal contraction force during manual testing: 4/5;
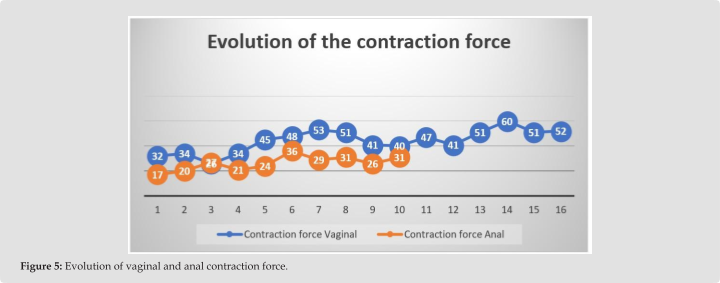
8. Vaginal contraction force by means of the probe and the Phenix device: 32 μv;
9. Anal contraction force during manual testing: 3/5;
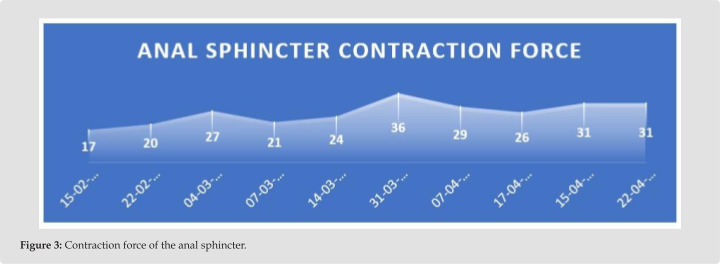
10. Anal contraction force by means of the probe and Phenix device: 17 μv.
Several perineal re-education techniques are put into practice: biofeedback and vaginal electrical stimulation for urinary inconti- nence, biofeedback and anal electrical stimulation for fecal inconti- nence, a specific protocol of exercises to train the pelvic floor muscles, awareness and systematic use of perineal blockage before an effort or sports gesture correlated with breathing, abdominal-lumbo-perineal muscle rebalancing, abdominal muscle training through hypopres- sive exercises, stretching exercises to maintain elasticity and relax the pelvic muscles. [26-28]. In the first session, manual recovery was performed for the understanding, awareness and correct execution of the contraction both at the beginning of the vaginal and anal sessions. Manual recovery takes about 20 minutes, during which the therapist performs manual muscle testing, checks tonicity, the presence of any asymmetry, pain, explains the anatomy, physiology of the pelvic floor and especially explains the correct way of perineal contraction. Sev- eral series of short contractions will be performed as well as contrac- tions with a minimum of 5 seconds of maintenance depending on the patient’s capabilities. Electrical stimulation associated with vaginal biofeedback using the Periform Plus vaginal probe and the Phenix Nano Physio-Uro perineal recovery device. The wireless electrostim- ulation and biofeedback technology allows rehabilitation to be car- ried out orthostatically and orthodynamically without cable-induced interference. The disappearance of the wires between the central unit and the patient simplifies the setting up of the session, and gives a lot of flexibility to the electrostimulation treatments which can now be integrated into exercise retraining exercises. Associated electrostim- ulation and biofeedback in patients who have difficulty integrating a motor pattern, the combination of stimulation and wireless biofeed- back can create a sensory-motor experience for a few seconds. The patient can easily reproduce the perineal locking reflex under bio- feedback in both orthostatic and orthodynamic.
Biofeedback trained slow-twitch fibers and fast-twitch fibers through brief maximal contractions and sub-maximal contractions with a 6-8 second hold. Also for bladder instability, the bladder in- hibition program with a frequency of 5 Hz associated with a biofeed- back program that triggers the A3 Mahony reflex was used. The pa- tient must be taught to anticipate the uninhibited contraction of the detrusor by a voluntary contraction of the pelvic floor. This activation of Mahony’s No. 3 reflex thus allows the patient to control his mictu- rition urges.
Program 1: “Mixed Urinary Incontinence- Muscle arousal and bladder inhibition” – 24 minutes per session; 5 sessions were performed in the lying position.
Program 2: “Mixed Urinary Incontinence – Phasic and tonic perineal contractions: EMS + Biofeedback” – 24 minutes per session; 10 sessions were performed. Thanks to the wireless probe, the patient performed the exercises on the gym ball, standing, lunging or squat- ting, standing on the BOSU top ball, on the bicycle, on the elliptical.
Anal recovery was performed using the Analys Plus anal probe with the aim of training the fast and slow fibers of the anal sphincter through electrical stimulation and biofeed- back. At the first session, manual recovery was performed for understanding, awareness and correct execution of the contraction, explaining the correct evacuation during defe- cation:
Program 1- Anal imperiousness
Program 2 – Tonic fiber awareness through isotonic and isometric
ESF + BFB
Recovery through physical exercises consisted of hypopressive pelvic-lobo-abdominal exercises. 4 exercise sessions were performed with perineal block explanation and learning, abdominal muscle strengthening performed after 10 biofeedback and EMS sessions, once perineal contraction was correctly learned and performed. The exercises were explained, performed and learned in the office, after which the patient will perform them at home 2.3 times a week. Ses- sions started in September 2021 to February 2022 – vaginally – 18 sessions vaginally, of which in the first session there was a manual recovery for understanding, awareness and correct execution of the contraction and 17 sessions with the Phenix Nano device and the probe vaginal Periform Plus. After 10 recovery sessions with electro- stimulation and biofeedback, once the perineal contraction was cor- rectly learned and performed, in November 2021, 4 physical exercise sessions were performed. The exercises were explained, performed and learned in the office, later the patient performed them at home
2.3 times a week to complement the training done in the office with the help of electrostimulation and biofeedback. The physical exercis- es consisted of training the abdominal muscles through the hypopres- sive method, short and slow contractions of the pelvic floor muscles in different positions simultaneously with the contraction of the abdom- inal muscles to train the perineal blocking reflex during abdominal hyperpressures. From February 2022 to April 2022, 11 anal sessions were performed. In the first session there was a manual recovery for the understanding, awareness and correct execution of the contrac- tion and 19 sessions with the Phenix Nano device and the Analys Plus anal probe. This case study has been approved by the UNEFS Bucha- rest Research Ethics Commission with number 104/25.01.2021. The patient gave her written consent for the production of this article with strict respect for anonymity.
During 4 months, 22 office sessions were performed for urinary incontinence associated with the home exercise protocol with a fre- quency of 1.2 times per week.

For anal incontinence associated with the home exercise protocol were performed 11 sessions with a frequency of 1.2 times per week for 3 months.
Table 1: Fecal incontinence – quality of life questionnaire – WIESEL.
|
Fecal incontinence – quality of life questionnaire – WIESEL |
||
|
Scor |
Quality of life percentage |
|
|
Initial |
43 |
34% |
|
Intermediate |
76 |
60% |
|
Final |
94 |
74% |
The re-education program was designed together with the patient and according to her. Because of her state of anxiety, discouragement, and worry, the first session consisted of understanding her condition history, fears, and setting priorities. We decided to start treatment with vaginal re-education to treat urinary incontinence first. The idea of vaginal recovery was initially easier to accept from a psychologi- cal point of view. Also, she had never performed an intra-vaginal or intra-anal kinetic treatment before. Intracavitary techniques require written consent from the patients stating that they can withdraw this consent at any time. Therefore, good communication, motivation and a relationship of trust between the patient and the therapist are nec- essary.
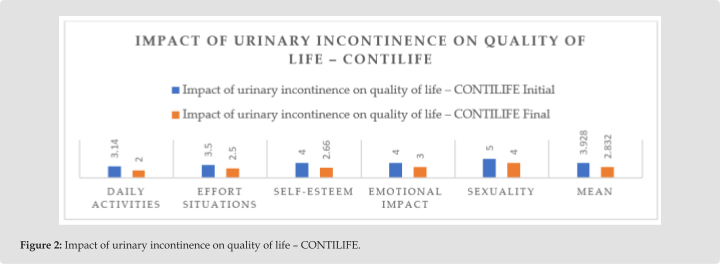
Given that urinary and fecal urges had the most important impact on the patient, she started in both vaginal and anal recoveries with programs to improve bladder hyperactivity, anal urges and slow-ton- ic fiber training. The patient states that the urges were so important that she could not get from the sofa to the toilet. The second stage of the recovery was to continue training the slow fibers but also add- ing the tonic-phasic and phasic fiber training programs. The sessions took place at a frequency of 1, 2 times a week in the office and ap- proximately 2 sessions of physical exercises at home. The pelvic floor muscle training with or without biofeedback or electrostimulation is reducing urinary incontinence and improve pelvic floor muscle con- traction [29]. The pelvic floor muscle training with behavioral thera- py and lifestyle modifications are effective first line treatments [30- 34]. This health problem proved to be a disabling handicap for the patient from a psychological, social and intimate point of view. She suffered from depression, job loss, increased smoking addiction and the inability to establish a married life. I noticed that, following the 6 months of physical therapy, the patient’s quality of life improved significantly, she has a married life, she manages to gradually regain her self-confidence, but the three years in which she suffered from severe urinary and fecal incontinence, from my point of view as a therapist, left psychological sequelae that should be treated by a spe- cialist. The Contilife questionnaire reveals that the impact of urinary incontinence on the quality of life decreased by an average of 22%, a percentage that is not exactly high although the frequency of uri- nary and fecal incontinence has decreased significantly, as the patient still presents increased anxiety related to this condition. Following discussions, she reports that she still answers the questions of the questionnaire with a rather high score because she anticipates that she might have incontinence in certain situations and often feels “a fragility and a perineal pressure” without necessarily having actual urinary leakage. This fragility or pressure declared by the patient can be a general ligament relaxation of the pelvic floor that causes a de- scent of the pelvic organs especially during certain physical activities. [35-36]. Also, this sensation could also be the feeling of the descent of the already existing prolapsus, which is accentuated especially during efforts and abdominal hyperpressures. In the long term, there is a risk
of relapse, that is why I recommend the patient to continue the pelvic and abdominal floor training exercises at least twice a week, so as to perform an annual medical check-up and possibly perform a series of 10 annual electrostimulation and biofeedback sessions for preven- tion relapses. It will be interesting to analyze the long-term results and evolution of the patient and to analyze a representative popula- tion who can generate more information on rates, ratios, incidences or prevalences.
Most of the time, urinary incontinence in sportswomen is not due to a hypotonia of the pelvic floor muscles, but rather the loss of the involuntary reflex and the perineal automatism to contract during the effort or, in some cases, it can be due to a muscle hypertonicity through which the perineal muscles do not have the ability to relax, thus leading to muscle exhaustion. Following the physiotherapy treat- ment, the symptoms were significantly reduced, the perineal muscle contraction force increased and the patient’s quality of life increased. However, the patient maintains a rather high anxiety related to uri- nary and fecal incontinence through the fear of having a job, being still unemployed, the fear of participating in certain activities, during sexual acts and especially the fear that the incontinence urine and fae- ces may return with the same intensity as at the beginning. In the long term, there is a risk of relapse, that is why I recommend the patient to continue the pelvic and abdominal floor training exercises at least twice a week, so as to perform an annual medical check-up and possi- bly perform a series of 10 annual electrostimulation and biofeedback sessions for prevention relapses. In conclusion physiotherapy is an ef- ficient treatment for urinary and fecal incontinence for a nulliparous young athlete and it should be one of the first treatment intentions.
The authors declare no conflict of interest.
Incontinence. Clinical obstetrics and gynecology 64(2): 306-313.

This work is licensed under Creative
Commons Attribution 4.0 License
Submission Link: https://biomedres.us/submit-manuscript.php
WhatsApp us