National University of Physical Education and Sports, Faculty of Physical Education and Sport, Romania.
*Corresponding author: Alexandra Tufa, National University of Physical Education and Sports, Faculty of Physical Education
and Sport, Bucharest, Romania
Corresponding author: alexandratufa@yahoo.com
Received: 4 June 2022 / Revised: 12 September 2022 / Accepted: 15 September 2022 /
Published: 30 September 2022
Copyright: © 2022 Tufa and Teodorescu. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Intense physical activity or certain branches of sport have many health benefits but can also have harmful effects on the pelvic floor. In medical literature, intensive exercise is mentioned as a risk factor for urinary incontinence by loss of anticipated cushion contraction during physical exertion, impairment of pelvic muscle tone and strength, lack of pelvic floor muscle relaxation, which may lead to muscle exhaustion, all of this causing a lack of response during the rapid increase of intra-abdominal pressure. This study aims to design a recovery protocol to reduce or eliminate symptoms of urinary incontinence in young female athletes affected by this condition through a complex approach to the rehabilitation of pelvic floor muscle tone and strength and specific training programmes to create a “perineal blockage”, the automatic contraction of pelvic floor muscles during physical exertion and relaxation at rest, the correction of both lumbar posture and muscle imbalance in the abdominal-lumbo-pelvic (core) area. The case studies included two patients, young female athletes aged 15 and 20, suffering from urinary incontinence. The methods used were: literature review, observation, questionnaire survey (Contilife questionnaire), graphical method, mathematical and statistical method. The results show that the symptoms of involuntary urine leakage have disappeared from the physiotherapy treatment of patients and their quality of life has increased. However, it is recommended that this exercise protocol be continued at home or introduced to sports training at least once a week to maintain the outcome and prevent recurrence.
Keywords: urinary incontinence, young female athletes, pelvic floor muscle exercises.
Urinary incontinence (UI) is defined as the involuntary loss of urine at an inappropriate time and in an inappropriate place (Burden et al., 2013), and epidemiological studies reveal that this condition is two or three times more frequent in women.
The most common forms of UI are typically classified as stress urinary incontinence (SUI), urge urinary incontinence (UUI) and mixed urinary incontinence (MUI).
Stress urinary incontinence (SUI) refers to involuntary leakage of urine during physical exertion (for instance, sports activities) or while sneezing/coughing. Urge urinary incontinence (UUI) involves unintentional loss of urine associated with urgency; this occurs due to a
condition called overactive bladder, whose symptoms are nocturnal urgency and frequency. Mixed urinary incontinence (MUI) combines SUI and UUI (Haylen et al., 2010).
In a systematic literature review (Milsom et al., 2017), the prevalence rate of urinary incontinence ranges from 24% to 45%, and SUI represents more than two-thirds of UI cases. This variation in prevalence is due to the use of different definitions of UI, data collection methods, response rates and investigated populations (Bø, 2020).
Risk factors for urinary incontinence are: age, body mass index, parity and mode of delivery
– where vaginal birth is the most important (Milsom et al., 2017). However, much lower prevalence rates of UI (12% to 13%) have been reported in large studies of nulliparous young women compared to female athletes, for whom the risk of UI is three times higher. The prevalence is generally increased in women performing high-impact sports (for example, running and jumping), but there is insufficient knowledge on women participating in weightlifting and other strength-demanding sports (Bø & Nygaard, 2020). A prevalence of 80% has been found in adolescent nulliparous trampoline jumpers (Eliasson et al., 2002). Given that SUI occurs during physical exertion, the activity level of the investigated population is a major factor to be taken into account when making a comparison between the results of prevalence studies and risk factors. “Mild-to-moderate physical activity, such as walking, decreases the risk of urinary incontinence but female athletes are about three times more likely to have urinary incontinence compared to controls.” (Bø & Nygaard, 2020, p. 471)
Women’s pelvic floor
Women’s pelvic floor is composed of three separate paired muscles, namely the pubococcygeus, puborectalis and iliococcygeus, which are attached to the pelvis as follows: anteriorly – pubic bodies of the pelvic bones; laterally – thickened fascia of the obturator internus muscle that is also known as the tendinous arch.
Pelvic floor muscles (PFM) form the lower part of the abdominal cavity on which the pelvic organs rest and through which the urethra, vagina and rectum pass; the area that surrounds the three openings of the female pelvic floor is called levator hiatus, being the largest hernia port in the body (Ashton-Miller & DeLancey, 2015). In pelvic organ prolapse, either the bladder, uterus or rectum, or all of these organs protrude through the vagina (DeLancey et al., 2008).
The pelvic floor contains three layers of muscles whose origins, insertions and fibre directions are different. Pelvic floor muscles have a constant activity, except just before and during voiding and defecation (Bø et al., 2017). If each pelvic floor muscle contracted separately, then each of them would have a different function; but the voluntary contraction of PFM involves a mass contraction that is observed as a squeeze around the openings and a lift of the pelvic floor in a forward and inward direction (Bø, 2007).
If the pelvic floor is functioning well, the connective tissue of ligaments and fasciae and the pelvic floor muscles work together to counteract the impact of any increase in intra-abdominal pressure and ground reaction forces, thus keeping the pelvic organs in place with little downward movements and little or no opening of the levator hiatus area or the urethra (DeLancey et al., 2008; Ashton-Miller & DeLancey, 2015). This function is automatic, which is why there is no need for women who lack symptoms and have a well-functioning pelvic floor to think about the voluntary PFM contraction. However, if these muscles do not work properly (for example, due to inherited or acquired factors), pelvic floor dysfunction is likely to occur (DeLancey et al., 2008; Ashton-Miller & DeLancey, 2015; Vodušek, 2015).
Pelvic floor dysfunction includes “urinary incontinence, anal incontinence, pelvic organ prolapse, sensory and emptying abnormalities of the lower urinary tract, defecatory dysfunction, sexual dysfunction and several chronic pain syndromes” (Bump & Norton, 1998, p. 723). These authors created a model describing possible aetiological factors in female pelvic floor dysfunction, which were classified as predisposing, inciting, promoting or decompensating.
DeLancey et al. (2008) subsequently developed this model into an integrated lifespan model. A graphical tool was used to integrate the factors affecting pelvic floor disorders and describe pelvic floor function in the following three key phases: “(1) development of functional reserve during an individual’s growth; (2) variations in the amount of injury and potential recovery that occur during and after vaginal birth; (3) deterioration that occurs with advancing age” (DeLancey et al., 2008, p. 610.E1).
Pelvic floor in female athletes
Numerous risk factors for urinary incontinence have been identified in the general population, including vaginal delivery, older age, obesity, diet, urinary infection, hormone disorders and chronic bronchitis. UI prevalence is variable in athletes and depends on the exercise intensity, movements performed and ground impact. For these individuals, the major cause seems to be an increase in abdominal pressure, which is followed by a contraction of abdominal muscles in the absence of a previous contraction of pelvic muscles.
According to a recent meta-analysis by Teixeira et al. (2018), the mean prevalence of UI is 36.1%, ranging from 19.4% to 76%, but these percentages refer to all-level female athletes. In professional female athletes, the risk of urinary incontinence seems to be about three times greater than in non-active women (Da Roza et al., 2015). Moreover, high-impact sports have been associated with an increased prevalence of UI compared to low-impact sports activities (80% versus 5.56%) (De Mattos Lourenco et al., 2018). This can be explained by the fact that high-impact sports are likely to produce higher intra-abdominal pressure, which leads to pelvic floor muscle weakness (Da Roza et al., 2015), morphological and functional changes in the connective tissue and ligaments (Fozzatti et al., 2012) or an increased diameter of the levator hiatus (Kruger et al., 2007). Therefore, the general belief that the pelvic floor of physically fit women is stronger due to regular exercise, which would prevent the development of UI, still needs to be questioned (Almousa & Bandin Van Loon, 2019).
Although some studies (Almeida et al., 2015; Carvalhais et al., 2018) reported the presence of UI in young athletes aged 15 years, the American College of Sports Medicine (2018) has not included it among the conditions that specifically affect women. Elite female athletes showed a high prevalence of UI, but this condition was also reported in male athletes. Despite this, only 9% of athletes reported current or past UI problems. This could indicate that urine leakage is often considered as either normal or a result of training demands. Thus, 29.1% said they had experienced loss of urine during the competition season, suggesting possible effects on their sports performance.
The study by Rodríguez-López et al. (2020) revealed that 33% of athletes aged 23.75 years on average had urinary incontinence. The prevalence of UI was 45.51% in female athletes and 14.7% in male athletes, meaning that women were 5.45 times more likely to be affected by this condition. (Figure 1)
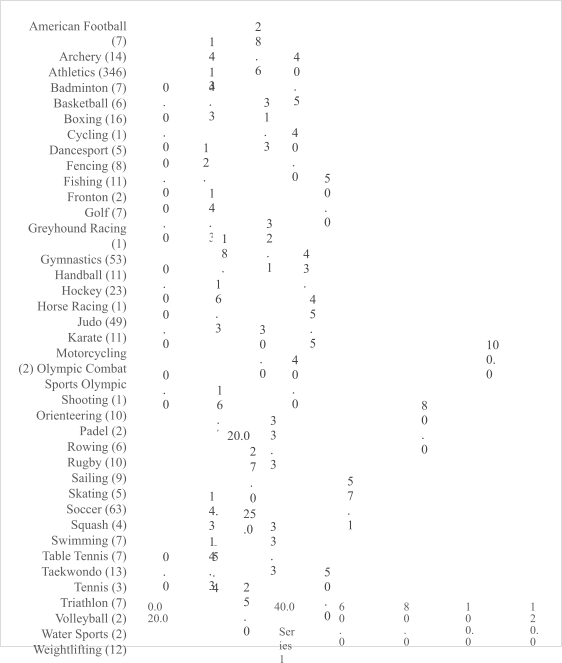
Figure 1. Prevalence of UI by sport (Rodríguez-López et al., 2020, p. 342)
Quality of life
According to Corcos et al. (2002), although urinary incontinence is not considered a severe disorder and does not have a direct impact on people’s lives, this condition is related to various psychological, social and economic problems. It is not a life-threatening issue but an embarrassing situation that has negative effects on the quality of life of individuals (De Mattos Lourenco et al., 2018). Even if urinary incontinence affects both genders, a higher prevalence is reported in women (51.1%) than men (13.9%) (Markland et al., 2011).
The loss of urine has serious consequences on the quality of life of adult women, affecting both their emotional state (Aslan et al., 2005; Virkud, 2011) and sexual intercourse (Kelleher, 2000; Saleh et al., 2005). Taking into account that urinary incontinence is related to body areas that are hidden by clothing and sexuality, it is still a taboo in many societies, being associated with myths and social restrictions (Roe & May, 1999). Thus, many women with UI often choose to stay home for fear and shame of losing urine in public, not finding a bathroom to change their clothes or protective pads when needed, etc. Therefore, they avoid going to parties or on long trips as well as performing physical activity (Kelleher, 2000; Saleh et al., 2005).
In the study by Lagro-Janssen et al. (1992), women reported that UI was not a problem to threaten their lives or restrict their daily activities, but it disturbed their lifestyles and especially their psychological functioning and well-being. Stach-Lempinen et al. (2003) investigated 82 women with UI and found that 26% had depressive symptoms, and 29% had anxiety symptoms. According to Yip and Cardozo (2007), psychological disorders are probably due to the impact of UI on an individual’s quality of life. Melville et al. (2002) as well as Vigod and Stewart (2006) suggest that major depression and comorbidity considerably affect quality of life for women with UI. Stach-Lempinen et al. (2003) highlighted that this category of women reported a decline in their quality of life and more symptoms of depression.
Coping strategies are crucial to maintain an individual’s identity and perceived competence (Peake & Manderson, 2003), given that UI is often associated with lack of self-control (Brittain & Shaw, 2007). Thus, active coping, accepting one’s own disorder, expressing one’s own feelings, being optimistic and showing positive religious coping are thought to increase quality of life. On the other hand, behavioural disengagement, self-blame, high distraction and negative religious coping (such as a pessimistic view of the world and spiritual discomfort) lead to a decline in quality of life for people with chronic diseases.
Jácome et al. (2011) state that UI negatively impacts the quality of life of female athletes. Considering the impact of UI on the daily life of elite athletes, this condition is likely to compromise their sports performance. It should be highlighted that more than half of the population surveyed in the above study were high-level athletes (participants in the Olympic Games, in World and European competitions), meaning that much of their day was dedicated to training. Their competition results may be affected since 29.1% of these top medallists indicated that they had experienced urine leakage during competition periods. In addition to the impact of UI on sports performance, athletes may experience feelings of concern and frustration that their urine leakage might be noticed by the people around them. Unfortunately, most athletes never discuss problems related to urine leakage with anyone or seek treatment. Professionals involved in their training should be aware of the implications of UI and refer them for physiotherapy support, if necessary.
Therefore, proper preventive and/or therapeutic strategies should be adopted for athletes with UI. First of all, their training volume needs to be examined. Current data in the literature indicate that weekly training hours have an influence on the development of UI, but this relationship is not very clear in terms of hours per day or years of training. The crucial point seems to be the break between workouts and weeks of rest during a year. Eliasson et al. (2005) believe that a different personal fatigue threshold should exist for each female athlete, thus suggesting that the continence mechanism may be affected when this threshold is exceeded.
The methods used in this investigation were: literature review, observation, questionnaire survey (Contilife questionnaire), graphical method and mathematical statistics, which were applied to two case studies.
The research was conducted in a physiotherapy clinic in Lyon, France, between October 2020 and February 2021, on two young female athletes suffering from urinary incontinence.
The first case was a 15-year-old female athlete experiencing stress urinary incontinence for many years. The second case was a 20-year-old female athlete experiencing urge urinary incontinence for about six months. Both young women were healthy, had no disease that could influence urine leakage (e.g., muscular dystrophy, genetic disorders affecting the connective tissue, no history of frequent urinary tract infections, no obesity) and had no surgery for urinary incontinence. The two patients benefited from 15 physiotherapy rehabilitation sessions and a home exercise protocol. They were very motivated to engage in the rehabilitation programme because urine leakage had a social, psychological and intimate impact on their lives (Table 1). During the rehabilitation programme, only the physical exercise method was used. Given their age, a non-invasive method was recommended. Biofeedback or electrostimulation (which is an intravaginal method) can be uncomfortable or harmful for young patients.
For the first session, due to intravaginal manual testing, patients under 18 years of age must be accompanied by a parent. All patients must sign a written consent on the physical therapy methods and an agreement on the information processing for scientific research purposes.
Table 1. Main information about the two patients
Variable | Patient 1 (SUI) | Patient 2 (UUI) |
Age | 15 | 20 |
Weight | 63 | 52 |
Height | 1.73 | 1.65 |
BMI (Body Mass Index) | 21 | 19 |
Sports | Gymnastics, Volleyball, Gym | Fitness, Crossfit |
Training – Hours/week | 6 Hours/week | 4 to 5 Hours/week |
Symptoms | Urine leakage | Urine leakage |
Since | 5 years | 6 months |
Type of UI | SUI | UUI |
Recovery motivation | Very motivated | Very motivated |
Recovery session before | No | No |
Information about the patient | Insufficient | Little information |
Rehabilitation sessions | 15 sessions | 15 sessions |
Frequency of rehabilitation sessions | 2/week | 1/week |
Home protocol exercises | Yes | Yes |
The strength training programme aims at developing muscles and improving structural support to counteract any increase in intra-abdominal pressure and ground reaction forces. Inpractice, pelvic floor training is proposed as a forefront treatment for women experiencing stress urinary incontinence.
Patients are recommended 10 up to 20 sessions if no subjective or identifiable clinical improvement is noticed. At the end of the first series of sessions, it should be considered whether physical therapy sessions need to be continued. If both the therapist and the patient observe that the improvement is inappropriate but present, the treatment can be extended to 20 sessions. If the patient believes that the improvement is acceptable or appropriate (subjective criteria) and if the objective assessment criteria indicate that the improvement or recovery is significant, then pelvic floor training can be stopped, with the advice to continue the protocol at home or include the exercises in the training programme. The literature review has highlighted that patient follow-up and self-management have beneficial effects over time.
According to ANAES (National Agency for Accreditation and Health Assessment) France (2000), pelvic floor muscle training (PFMT) in urinary incontinence can only begin after performing an initial examination based on which the therapist selects the techniques, monitors changes in symptoms and measures rehabilitation outcomes.
By checking the patient’s history, the therapist will seek to find different types of information in order to define a treatment strategy:
All these factors are used to develop a comprehensive patient management strategy. Clinical examination is focused on:
All these involve several stages aimed at:
Even though strength measurement is subjective and its reproducibility has not yet been assessed, this test is largely used by professionals to reflect the quality of muscle contraction and the patient’s ability to use the muscle system with or without contracting other muscles. The same pelvic floor evaluation protocol should always be used for any patient before, during and after treatment. The purpose of muscle testing is to assess pelvic floor muscle strength and endurance and detect any possible disorder in the control sequence. It is both an aid for the selection of pelvic floor training techniques and an indicator for monitoring muscle contractility
(strength, endurance). It is used to assess the improvement of muscle strength rather than the effectiveness of pelvic floor training.
Table 2. Modified Oxford Pelvic Tone Scoring System (Price et al., 2010)
Oxford Score | Signs |
0 | No contraction |
1 | A flicker |
2 | Weak |
3 | Moderate with some lift |
4 | Good contraction with lift against some resistance |
5 | Normal muscle contraction, strong squeeze and lift |
The exercises comply with the muscle training principles of painless and progressivity and combine long and short contractions in static and dynamic positions while practising under pressure exertion conditions. Some exercises are part of a self-rehabilitation programme based on the needs and individual progression of the patient.
The exercise protocol is structured as follows:
In the first part of recovery, which includes exercises for pelvic floor strengthening, no materials are needed (a floor mat is enough). The patient is advised to do the protocol at home for 30 minutes per day, three times a week.
In the middle part of recovery, some dynamic exercises are added, such as using a fit ball or different walking, running, cycling or stepper exercises. The patient has to combine long and short contractions during dynamic exercises.
The final part of recovery includes high-impact ground exercises, trampoline, skipping rope and some exercises from the patient’s training that cause urine leakage.
The home exercise protocol will be provided and explained by the physiotherapist in the first session. These exercises do not require specific material. Patients will apply pelvic floor and core muscle contraction during their daily activities and training sessions. Additional information and explanations can be provided on patient’s request.
Results show a decreased impact of urinary incontinence on patients’ lives and an improvement in their quality of life.
After rehabilitation, in the first subject we noticed the disappearance of urinary leakage and a complete improvement of the of UI life impact from a social and intimate point of view. On the other hand, from a psychological point of view, the impact decreased from 66% to 33%, the patient stating that there was still a fear that this problem may be reccurent. We also noticed an improvement in the quality of life of: 0.21 in daily activities, 0.50 in daily efforts, 0.28 in terms of the impact of self-image and a 0.43 improvement of emotional consequences, respectively.
After rehabilitation, the second subject highlighted an improvement of a UI life impact from a social point of view by 0.33, while in the case of the intimate impact the improvement was by 0.66; also, a removal of the psychological consequences was observed. Regarding the quality of life, assessed by the Contilife questionnaire, after rehabilitation, an improvement of 0.31 was found in daily activities, 0.21 in impact on self-image, 0.42 in terms of emotional consequences and minimizing daily efforts (Tables 3 and 4).
Table 3. UI life impact
UI life impact | ||||
Patient 1 (SUI) | Patient 2 (UUI) | |||
Before | After | Before | After | |
Social Impact | 0.66 | 0 | 0.66 | 0.33 |
Psychological Impact | 0.66 | 0.33 | 1 | 0 |
Intimate Impact | 0.33 | 0 | 1 | 0.33 |
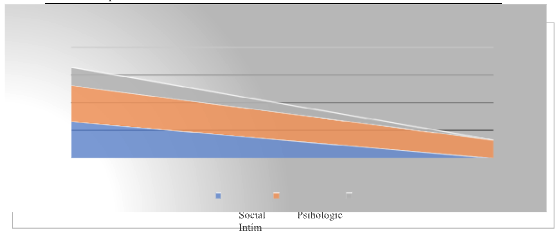
Figure 1. UI life impact
Table 4. Quality of life (Contilife) of patients before and after the rehabilitation programme
Quality of life (Contilife) | ||||
Patient 1 (SUI) | Patient 2 (UUI) | |||
Before | After | Before | After | |
Daily Activities | 0.28 | 0.07 | 0.37 | 0.05 |
Effort-Demanding Activities | 0.56 | 0.06 | 0.1 | 0 |
Self-Image Impact | 0.35 | 0.07 | 0.28 | 0.07 |
Emotional Consequences | 0.55 | 0.12 | 0.5 | 0.08 |
The studies presented in the specialized literature have emphasized an improvement of up to 70% in stress incontinence symptoms after correctly performing pelvic floor exercises. This improvement occurs across all age groups. Evidence shows that women have better performance when the exercise is guided by specialised physical therapists or continence nurses versus independent or leaflet-based care. Prescribing physicians and physiotherapists have a crucial role in the preparation of women for pelvic floor training and in-patient compliance (Price et al., 2010).
According to Bø and Sundgot-Borgen (2010), functional PFM training uses exercises that integrate an appropriate PFM contraction during everyday activities such as lifting, sneezing or training. This requires the patient to think of the PFM contraction throughout the day. However, it has not been proven that this would lead to an automatic behaviour or that pelvic floor muscle training based on functional training would have higher effectiveness than a properly dosed strength training programme alone. Considering that PFM strength training has a very good effect, a larger sample should be examined to highlight any extra benefit of using adjuvants, for instance, biofeedback or other exercise modalities.
Patients should be informed about the role of PFM, muscle testing, intravaginal techniques and the importance of rehabilitation. Patient management involves not only specific training but also good communication between the therapist and the patient. Listening to and understanding the patient’s problems is the first step to successful recovery treatment. We need to win the trust of our patients so that they can easily continue their sessions instead of giving them up.
However, some questions remain about the best PFMT programme to recommend if exercise alone is not enough to treat UI symptoms. Also, many issues raised in the current study have not yet been answered and can be considered as proposals for action. The critical aspects that need further research are:
The purpose of this paper was to investigate two patients, young female athletes diagnosed with urinary incontinence, as regards the recommended muscle strengthening programmes intended to treat their stress or mixed urinary incontinence.
The present study also aimed at identifying and proposing an effective rehabilitation programme solely based on exercises for pelvic floor strengthening in order to reduce urinary incontinence symptoms, improve the quality of life (Contilife) and diminish the social, psychological and intimate impact of UI on patients’ lives. The review of the study report certifies that PFM exercise is beneficial for treating stress urinary incontinence in women. Both patients had no more urine leakage after the rehabilitation programme.
According to the results of this study, the urine leakage symptoms of the two young female athletes have completely disappeared, the UI life impact has been reduced for both of them, and their quality of life has increased.
Evidence shows that PFM exercise is helpful for any type of female urinary incontinence. The present study allows us to recommend an optimal muscle training programme to treat urinary incontinence in women. Due to its effectiveness, pelvic floor rehabilitation can be used as a forefront treatment of urinary incontinence in young female athletes.
Professionals involved in patient training need to be aware of the UI implications and include pelvic floor muscle exercises in their training programmes.
Authors’ Contribution: Both authors have equally contributed to this study.
Funding: This research received no external funding.
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the National University of Physical Education and Sports in Bucharest, Romania (ID: 104).
Informed Consent Statement: The patients/participants provided their written informed consent to participate in this study.
Data Availability Statement: Data are available upon request to the contact author.
Conflicts of Interest: The authors declare no conflict of interest.
Almeida, M. B. A., Barra, A. A., Saltiel, F., Silva-Filho, A. L., Fonseca, A. M. R. M., & Figueiredo, E. M. (2015). Urinary incontinence and other pelvic floor dysfunctions in female athletes in Brazil: A cross-sectional study. Scandinavian Journal of Medicine & Science in Sports, 26(9), 1109-1116. https://doi.org/10.1111/sms.12546
Almousa, S., & Bandin Van Loon, A. (2019). The prevalence of urinary incontinence in nulliparous female sportswomen: A systematic review. Journal of Sports Sciences, 37(14), 1663-1672. https://doi.org/10.1080/02640414.2019.1585312
American College of Sports Medicine. (2018). Female athlete issues for the team physician: A consensus statement – 2017 update. Medicine & Science in Sports & Exercise, 50(5), 1113- 1122. doi: 10.1249/MSS.0000000000001603
Ashton-Miller, J., & DeLancey, J. O. L. (2015). Functional anatomy of the female pelvic floor. In K. Bø et al. (Eds.), Evidence-based physical therapy for the pelvic floor. Bridging Science and Clinical Practice (Chapter 3, pp. 19-34). Churchill Livingstone. https://doi.org/10.1016/B978-0-7020-4443-4.00003-0
Aslan, G., Köseoğlu, H., Sadik, Ã., Gimen, S., Cihan, A., & Esen, A. (2005). Sexual function in women with urinary incontinence. International Journal of Impotence Research, 17(3), 248-251. https://doi.org/10.1038/sj.ijir.3901296
Bø, K. (2020). Physiotherapy management of urinary incontinence in females. Journal of Physiotherapy, 66(3), 147-154. https://doi.org/10.1016/j.jphys.2020.06.011
Bø, K., & Nygaard, I. E. (2020). Is physical activity good or bad for the female pelvic floor? A narrative review. Sports Medicine, 50, 471-484.
https://doi.org/10.1007/s40279-019-01243-1
Bø, K., & Sundgot-Borgen, J. (2010). Are former female elite athletes more likely to experience urinary incontinence later in life than non-athletes? Scandinavian Journal of Medicine & Science in Sports, 20(1), 100-104. https://doi.org/10.1111/j.1600-0838.2008.00871.x
Bø, K., Frawley, H. C., Haylen, B. T., Abramov, Y., Alemida, F. G., Berghmans, B., Bortolini, M., Dumoulin, C., Gomes, M., McClurg, D., Meijlink, J., Shelly, E., Trabuco, E., Walker, C., & Wells, A. (2017). An International Urogynecological Association (IUGA)/ International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurology and Urodynamics, 36(2), 221-244. https://doi.org/10.1002/nau.23107
Bø K. (2007). Pelvic floor muscle training for stress urinary incontinence. In: Bø K, Berghmans B, Morkved S, Kampen MV, editors. Evidence-based physical therapy for the pelvic floor. Philadelphia: Churchill Livingstone; 2007. p. 171-86
Brittain, K. R., & Shaw, C. (2007). The social consequences of living with and dealing with incontinence: A carers perspective. Social Science & Medicine, 65(6), 1274-1283. https://doi.org/10.1016/j.socscimed.2007.04.002
Bump, R. C., & Norton, P. A. (1998). Epidemiology and natural history of pelvic floor dysfunction. Obstetrics and Gynecology Clinics of North America, 25(4), 723-746. https://doi.org/10.1016/s0889-8545(05)70039-5
Burden, H., Warren, K., & Abrams, P. (2013). Diagnosis of male incontinence. Current Opinion in Urology, 23(6), 509-514. https://doi.org/10.1097/01.mou.0000434593.87575.e8 Carvalhais, A., Natal Jorge, R., & Bø, K. (2017). Performing high-level sport is strongly associated with urinary incontinence in elite athletes: a comparative study of 372 elite
female athletes and 372 controls. British Journal of Sports Medicine, 52(24). http://dx.doi.org/10.1136/bjsports-2017-097587
Corcos, J., Beaulieu, S., Donovan, J., Naughton, M., & Gotoh, M. (2002). Quality of life assessment in men and women with urinary incontinence. Journal of Urology, 168(3), 896- 905. https://doi.org/10.1097/01.ju.0000024401.79394.21
Da Roza, T., Brandão, S., Mascarenhas, T., Jorje, N. R., & Duarte, J. A. (2015). Urinary incontinence and levels of regular physical exercise in young women. International Journal of Sports Medicine, 36(9), 776-780. https://doi.org/10.1055/s-0034-1398625
De Mattos Lourenco, T. R., Katsumi Matsuoka, P., Baracat, E. C., & Haddad, J. M. (2018). Urinary incontinence in female athletes: A systematic review. International Urogynecology Journal, 29(12), 1757-1763. https://doi.org/10.1007/s00192-018-3629-z
DeLancey, J. O. L. (1997). The pathophysiology of stress urinary incontinence in women and its implications for surgical treatment. World Journal of Urology, 15(5), 268-274. https://doi.org/10.1007/bf02202011
DeLancey, J. O. L., Kane Low, L., Miller. J. M., Patel, D. A., & Tumbarello, J. A. (2008). Graphic integration of causal factors of pelvic floor disorders: An integrated life span model. American Journal of Obstetrics and Gynecology, 6, 610.E1-610.E5 https://doi.org/10.1016/j.ajog.2008.04.001
Eliasson, K., Larsson, T., & Mattsson, E. (2002). Prevalence of stress incontinence in nulliparous elite trampolinists. Scandinavian Journal of Medicine & Science in Sports, 12(2), 106-110. https://doi.org/10.1034/j.1600-0838.2002.120207.x
Eliasson, K., Nordlander, I., Larson, B., Hammarstöm, M., & Mattsson, E. (2005). Influence of physical activity on urinary leakage in primiparous women. Scandinavian Journal of Medicine & Science in Sports, 15(2), 87-94.
https://doi.org/10.1111/j.1600-0838.2004.407.x
Jácome, C., Oliveira, D., Marques, A., & Sá-Couto, P. (2011). Prevalence and impact of urinary incontinence among female athletes. International Journal of Gynecology & Obstetrics, 114(1), 60-63. https://doi.org/10.1016/j.ijgo.2011.02.004
Kelleher, C. (2000). Quality of life and urinary incontinence. Best Practice & Research Clinical Obstetrics & Gynaecology, 14(2), 363-379. https://doi.org/10.1053/beog.1999.0079
Kruger, J. A., Dietz, H. P., & Murphy, B. A. (2007). Pelvic floor function in elite nulliparous athletes. Ultrasound in Obstetrics & Gynecology, 30(1), 81-85. https://doi.org/10.1002/uog.4027
Lagro-Janssen, T., Smits, A., & Weel, C. V. (1992). Urinary incontinence in women and the effect on their lives. Scandinavian Journal of Primary Health Care, 10(3), 211-216.
Markland, A. D., Richter, H. E., Fwu, C.-W., Eggers, P., & Kusek, J. W. (2011). Prevalence and trends of urinary incontinence in adults in the United States, 2001 to 2008. The Journal of Urology, 186(2), 589-593. https://doi.org/10.1016/j.juro.2011.03.114
Melville, J. L., Walker, E., Katon, W., Lentz, G., Miller, J., & Fenner, D. (2002). Prevalence of comorbid psychiatric illness and its impact on symptom perception, quality of life, and functional status in women with urinary incontinence. American Journal of Obstetrics & Gynecology, 187(1), 80-87. https://doi.org/10.1067/mob.2002.124839
Milsom, I., Altman, D., Cartwright, R., Lapitan, M. C., Nelson, R., Sjöström, S., & Tikkiten,
Peake, S., & Manderson, L. (2003). The constraints of a normal life: The management of urinary incontinence by middle aged women. Women & Health, 37(3), 37-51. https://doi.org/10.1300/j013v37n03_03
Price, N., Dawood, R., & Jackson, S. R. (2010). Pelvic floor exercise for urinary incontinence: A systematic literature review. Maturitas, 67(4), 309-315. https://doi.org/10.1016/j.maturitas.2010.08.004
Rodríguez-López, E. S., Calvo-Moreno, S. O., Basas-García, Á., Gutierrez-Ortega, F., Guodemar-Pérez, J., & Acevedo-Gómez, M. B. (2020). Prevalence of urinary incontinence among elite athletes of both sexes. Journal of Science and Medicine in Sport, 24(4), 338-
Roe, B., & May, C. (1999). Incontinence and sexuality: Findings from a qualitative perspective.
Journal of Advanced Nursing, 30(3), 573-579. https://doi.org/10.1046/j.1365-2648.1999.01126.x
Saleh, N., Bener, A., Khenyab, N., Al-Mansori, Z., & Muraikhi, A. A. (2005). Prevalence, awareness and determinants of health care-seeking behavior for urinary incontinence in Qatari women: A neglected problem? Maturitas, 50(1), 58-65.
https://doi.org/10.1016/j.maturitas.2004.04.003
Stach-Lempinen, B., Hakala, A.-L., Laippala, P., Lehtinen, K., Metsänoja, R., & Kujansuu, E. (2003). Severe depression determines quality of life in urinary incontinent women. Neurology & Urodynamics, 22(6), 563-568. https://doi.org/10.1002/nau.10137
Vigod, S. N., & Stewart, D. E. (2006). Major depression in female urinary incontinence.
Psychosomatics, 47(2), 147-151. https://doi.org/10.1176/appi.psy.47.2.147
Virkud, A. (2011). Management of stress urinary incontinence. Best Practice & Research Clinical Obstetrics & Gynaecology, 25(2), 205-216. https://doi.org/10.1016/j.bpobgyn.2010.10.013
Vodušek, D. B. (2015). Neuroanatomy and neurophysiology of pelvic floor muscles. In K. Bø et al. (Eds.), Evidence-based physical therapy for the pelvic floor. Bridging Science and Clinical Practice (Chapter 4, pp. 35-43). Churchill Livingstone. https://doi.org/10.1016/B978-0-7020-4443-4.00004-2
Yip, S.-K., & Cardozo, L. (2007). Psychological morbidity and female urinary incontinence.
Best Practice & Research Clinical Obstetrics & Gynaecology, 21(2), 321-329. https://doi.org/10.1016/j.bpobgyn.2006.12.002
WhatsApp us